
Physician well-being, AI momentum, and early exits among advanced practitioners are shifting clinical workforce dynamics. Our Q2 2025 Healthcare Market Report explores these trends and their impact on healthcare.
Complete the short form below for an in-depth look at the insights and trends impacting healthcare this quarter.
Locum Tenens Remains the Lone Bright Spot Within Temporary Staffing
The locum tenens market expanded by approximately 15% in 2024, driven by both bill rates and patient volumes. The segment is projected to grow 6% in 2025 and a 5% anticipated growth in 2026. In contrast, the nursing and allied health sectors, which peaked from 2020 to 2022, are now trending back toward pre-pandemic levels, based on data from Staffing Industry Analysts (SIA). 
According to SIA, the primary drivers of growth within the locum tenens segment include rising patient volumes, increased demand for procedures due to the aging population, and a broader range of health conditions for all ages.
AI in Practice: Growing Physician Confidence and Health System Investment
Reducing administrative burden remains a top priority for physicians, and AI is quickly emerging as a key part of the solution. Confidence in the technology is also growing: 35% reported feeling more excited than concerned about health AI, up from 30% the previous year, according to an AMA survey.


Health systems are actively integrating AI into clinical and operational workflows. A McKinsey & Company survey of 150 healthcare organizations found that 40% have already implemented generative AI. Nearly half (44%) of the survey respondents expect AI to improve administrative efficiency.
Early Exits: Rising Attrition of NPs and PAs in the ED
As emergency medicine physician shortages persist, many emergency departments have turned to nurse practitioners and physician assistants to maintain access to care. However, a new challenge is emerging with NPs and PAs leaving emergency medicine at notably higher rates and at younger ages, according to a study published in the Annals of Emergency Medicine. 
The study found a weighted annual attrition rate of 13.8% among NPs and PAs, with NPs exiting at higher rates than their PA counterparts. With emergency care demand on the rise and the physician pipeline constrained, these findings point to a growing need to retain experienced clinicians in the field.
Closing Provider Shortages: Strategies That Work
A recent Becker's Healthcare webinar, presented in partnership with Medicus, featured executives from Corewell Health and Trinity Health of New England. The discussion focused on how their organizations are navigating today’s complex workforce challenges and staffing shortages.
During the session, attending healthcare leaders participated in a live poll identifying the most difficult specialties to staff within their organizations: 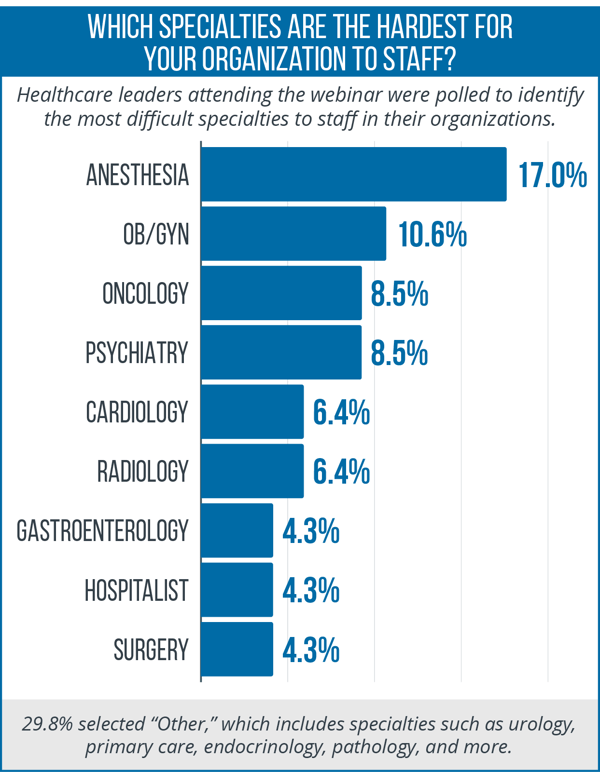
The conversation also highlighted key drivers behind the shortage, including an aging clinical workforce, rising procedural demand, shifting demographics, limitations in the training pipeline, and a growing preference among physicians for flexible schedules.
To respond effectively, both executives emphasized the need for structured workforce planning. Their approaches are designed to meet immediate operational demands while aligning with long-term organizational goals.
For a comprehensive look at these insights and additional trends shaping healthcare this quarter, download our Q2 Healthcare Market Report.


