2026 Healthcare Trends: A Guide for C-Suite Executives

In 2026, healthcare leaders will continue to face physician shortages amid rising patient demand and increasing operational pressure. The trends below highlight where challenges persist and where leaders can gain insight to protect access to care and maintain workforce stability.
Physician Workforce Shortages Will Continue to Strain Care Delivery
The clinical workforce continues to experience the effects of sustained demand, burnout, and staffing instability. While these pressures are not new, they are becoming harder to absorb as patient needs grow more complex, driven by an aging population, higher acuity, and shifting patient expectations.
Workforce projections suggest these shortages will intensify as retirements accelerate. While growth among physician assistants and nurse practitioners may help offset some gaps, these trends do not fully address the day-to-day realities of clinical workload across care settings.
In 2026, the United States is projected to see a shortage of 96,430 FTE physicians, according to projections from the Health Resources and Services Administration (HRSA), with uneven impact across specialties and regions.
Specialties Seeing the Highest Physician Shortages:
The following specialties are projected to experience the largest supply–demand gaps in 2026.
- Hospital Medicine: -5,350 FTEs
- Anesthesiology: -3,720 FTEs
- Cardiology: -3,010 FTEs
- Vascular Surgery: -2,170 FTEs
- General Surgery: -2,020 FTEs
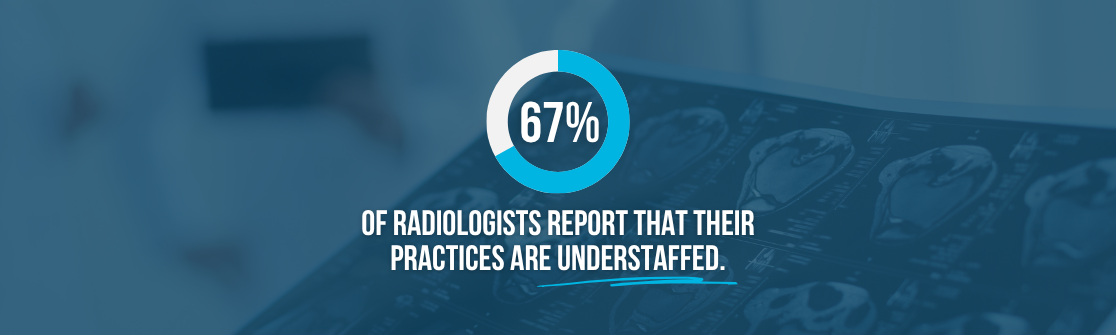
- Radiology: -1,900 FTEs
U.S. States with the Highest Physician Shortages:
The following states are projected to have the widest gaps between physician supply and demand in 2026 as of December 23, 2025.
- Florida: -18,370 FTEs
- Texas: -12,720 FTEs
- Georgia: -8,360 FTEs
- Arizona: -6,980 FTEs
- Indiana: -6,380 FTEs
- Tennessee: -6,260 FTEs
Operational Impact on Healthcare Organizations:
For healthcare organizations, these specialty shortages translate into operational complexities. Extended hiring timelines, a more competitive recruiting environment, rising compensation expectations, and the potential for service disruption are expected to continue. In this environment, locum tenens providers play an increasingly important role—not simply to address short-term gaps, but as a reliable part of a long-term workforce strategy.
 Source: Advisory Board, HRSA
Source: Advisory Board, HRSA
Rapid Advanced Practice Provider Growth is Reshaping Clinical Coverage and Access
Advanced practice providers (APPs) are projected to be among the fastest-growing segments of the clinical workforce. The U.S. Bureau of Labor Statistics projects 40% growth in nurse practitioner roles and 20% growth in physician assistant roles between 2024 and 2034. This growth reflects the increasing reliance on APPs to maintain access to care as physician shortages continue to challenge healthcare organizations.
Several factors are accelerating reliance on APPs, including:
- Ongoing physician retirements across multiple specialties
- An aging population with more chronic and complex care needs
- The ongoing challenge of maintaining access while controlling costs
As physician shortages persist, healthcare leaders can expect continued growth in demand for advanced practice providers in 2026. APPs, alongside locum tenens providers, will be essential to maintaining patient access and continuity of care as organizations navigate workforce constraints, fluctuating demand, and ongoing pressure on clinical capacity.
 Source: U.S. Bureau of Labor Statistics
Source: U.S. Bureau of Labor Statistics
Rural Hospital Closures Will Increase Pressure on Regional Health Systems
Rural hospitals continue to operate under significant financial pressure, with margins well below the national median and a growing share at immediate risk of closure. Rising costs, declining rural populations, reimbursement shifts toward Medicare Advantage, and potential changes to Medicaid funding are contributing to strain on the rural hospital business model. As a result, more than 700 rural hospitals are at risk of closure nationwide, including over 300 facing immediate risk due to severe financial challenges.
As these closures occur, their impact extends beyond rural communities. Closures are associated with reduced access to primary care, increased reliance on nearby emergency departments, and longer lengths of stay for emergency conditions at urban hospitals. Over time, these patterns place additional pressure on capacity, costs, and patient experience across regional care networks.
Some health systems and regional stakeholders are exploring partnership models as alternatives to acquisition to help preserve access and stabilize care delivery, such as regional call models. These approaches may support certain communities, but do not fully offset the broader erosion of the rural healthcare safety net.
For healthcare leaders, rural hospital closures represent a regional issue with implications for access, utilization, and system performance that are likely to remain relevant in 2026.
 Source: Advisory Board
Source: Advisory Board
AI Implementation Is Accelerating Across Healthcare
AI adoption is expected to accelerate as healthcare leaders increasingly view it as a tool to manage complexity, improve efficiency, and support care delivery amid ongoing financial and workforce pressure. While uncertainty remains across the industry, AI is becoming a central focus for organizations working to modernize operations and adapt to evolving care needs.
Healthcare leaders expect AI to deliver value across multiple areas, including:
- Clinical care, such as diagnostics, imaging, and clinical decision support
- Administrative and operational workflows, including documentation and revenue cycle processes
- Consumer and workforce experiences through AI-enabled tools and automation
Taken together, these signals point to 2026 as a transition year, with organizations moving from experimentation toward more disciplined, scalable AI use across the enterprise.
 Source: Deloitte 2026 U.S. Health Care Outlook Survey
Source: Deloitte 2026 U.S. Health Care Outlook Survey
Investing in Culture Will Be a Top Priority
As workforce expectations around flexibility and work-life balance continue to evolve, organizational culture is becoming a defining factor in physician recruitment and retention. This shift is being accelerated by a new generation of physicians entering practice with different expectations around work, autonomy, and organizational support. In a market shaped by persistent physician shortages, compensation alone is no longer sufficient to sustain the workforce.
Many physicians are increasingly prioritizing environments that offer manageable workloads, flexibility, and a culture that supports well-being alongside clinical excellence. These shifts are showing up in how physicians evaluate potential employers. Expectations around flexibility and work-life balance are rising, greater weight is being placed on the day-to-day work environment and organizational support, and competition for physicians remains intense across nearly all specialties.
While compensation remains a baseline expectation, culture is playing a larger role in retention decisions. 70% of physicians say organizational culture is just as important as compensation, positioning culture as a key differentiator in a constrained labor market.
Aligning Workforce Strategy for the Year Ahead
The workforce challenges shaping 2026 are unlikely to be resolved quickly. What will differentiate healthcare organizations is how intentionally they plan for variability across specialties, regions, and care settings.
As leaders assess their staffing approach for the year ahead, flexibility, foresight, and partnership are becoming increasingly important. Workforce strategies that account for both immediate coverage needs and longer-term stability are better positioned to protect access, support care teams, and sustain performance.
Partnering early with a locum tenens agency like Medicus can help healthcare leaders prepare for a range of workforce scenarios. This includes traditional locum tenens staffing, contingency planning for coverage disruptions, and staffing transitions designed to strengthen long-term stability through the Medicus Transition Program.
As clinical workforce pressures continue to evolve, investing now in a flexible, long-term staffing strategy can better position organizations to maintain patient access, support care teams, and navigate uncertainty in 2026 and beyond.
Interested in partnering with Medicus for locum tenens staffing? Complete the short form below to connect with a member of the Medicus team.