Insights Into the OB/GYN Shortage: Understanding the Supply and Demand Gap

OB/GYN workforce constraints continue to challenge healthcare organizations across the United States. Data published in the Association for Advancing Physician and Provider Recruitment's (AAPPR) 2024 Benchmarking Report found that over 60% of healthcare organizations reported conducting at least one search for a permanent OB/GYN (general), placing it among the top five most commonly recruited specialties nationwide.
OB/GYN hiring challenges are expected to persist, with the Health Resources and Services Administration projecting that by 2037, the United States will only meet 82% of the anticipated demand for OB/GYNs. As workforce numbers continue to decline, access to maternity care will become more limited, especially in rural areas where labor and delivery unit closures are accelerating.
Factors Contributing to the OB/GYN Supply & Demand Imbalance
Limited Growth in Residency Positions
While OB/GYN residency programs continue to attract strong applicant interest, the number of available positions has not kept pace with the increasing need for clinicians in the specialty. According to the National Resident Matching Program (NRMP), the number of PGY-1 obstetrics-gynecology positions has increased by an average of 2% annually since 2021, adding 127 positions over the four-year period.
Despite this modest growth, many qualified applicants are competing for a limited number of training opportunities. In the 2025 Match, 2,151 applicants competed for 1,587 PGY-1 OB/GYN positions. With a 99.9% fill rate, 564 applicants did not match into residency, delaying their entry into the specialty or redirecting them into other fields. Without a greater expansion of training capacity, the demand for OB/GYN services will continue to outpace the available workforce.

Heightened Burnout Rates Among OB/GYNs
Burnout remains a prevalent challenge across the physician workforce, and OB/GYNs are no exception. In a 2025 Medscape survey, nearly 30% of OB/GYNs reported being burned out, and 23% reported experiencing both burnout and depression.
One factor fueling burnout rates is the decline in work-life balance. In the same survey, 40% of OB/GYNs reported that their work-life balance had worsened over the past three years, and 66% indicated that they would accept a pay cut in exchange for improvement. Targeted strategies to enhance work-life balance and mitigate burnout will be crucial to attracting and retaining OB/GYN physicians. 
The Impact on Maternity Care Access
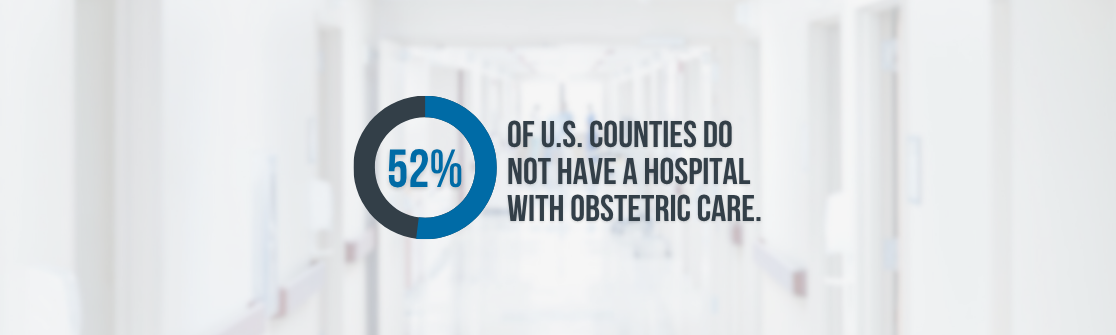
Between 2010 and 2022, over 500 hospitals in the U.S. closed their obstetric units, with rural hospitals accounting for more than 200 of those closures, according to a study published by the JAMA Network. This trend is continuing in 2025, with the number of rural labor and delivery hospitals that have closed or announced closures in the first half of the year already nearly matching the total for all of 2024, according to the Center for Healthcare Quality and Payment Reform.
These closures are contributing to the expansion of maternity care deserts, areas where access to obstetric care is limited or nonexistent. According to a 2024 report from the March of Dimes, more than 5.5 million women now live in counties with no or limited access to maternity care services, and over one-third of U.S. counties meet the criteria for a maternity care desert.
Actionable Solutions to Strengthen OB/GYN Coverage
Healthcare organizations are exploring and implementing various strategies to sustain OB/GYN services amid ongoing shortages and service line closures.
Incorporate an OB Hospitalist Model
One proven approach is implementing an OB hospitalist model, which ensures that a full-time or part-time physician is dedicated exclusively to inpatient obstetric care. This staffing model allows outpatient OB/GYNs to focus on clinical visits and elective procedures, while hospitals maintain uninterrupted, specialized coverage for labor, delivery, and obstetric emergencies.
Leverage Locum Tenens OB/GYNs
Locum tenens OB/GYNs are another vital resource for maintaining access to maternity care, particularly in rural and underserved communities where recruitment challenges are most acute. OB/GYN locum tenens can be mobilized quickly to stabilize staffing levels, cover unplanned vacancies, and maintain operational continuity in labor and delivery units.
Locum tenens OB/GYNs can also be integrated into a deliberate staffing strategy to ease pressures on permanent staff by redistributing workloads and providing protected time off. By leveraging OB/GYN locum tenens in this way, health systems can safeguard the well-being of the core OB/GYN team while strengthening retention and enhancing recruitment in a highly competitive labor market.
Utilize the Medicus Transition Program
For healthcare organizations facing multiple FTE gaps in coverage, the Medicus Transition Program can help. Medicus' project-based interim healthcare staffing solution specializes in long-term locum tenens coverage. By combining immediate locum tenens staffing support with strategic workforce planning, Medicus helps hospitals maintain reliable coverage and meet patient demand while helping build a more sustainable clinical workforce.
Explore More Insights into the OB/GYN Shortage
As the OB/GYN shortage continues to impact healthcare organizations, patients, and OB/GYNs alike, leveraging actionable staffing strategies will be crucial for maintaining and managing access to obstetrics and gynecological care. Our report, Insights into the Growing OB/GYN Shortage, provides a comprehensive look into the workforce, additional factors influencing the shortage, and an in-depth look into solutions for navigating it.
For a comprehensive look into the OB/GYN shortage, download the complete report below.