Navigating the Radiologist Shortage: Strategies for Meeting the Rising Demand in Healthcare
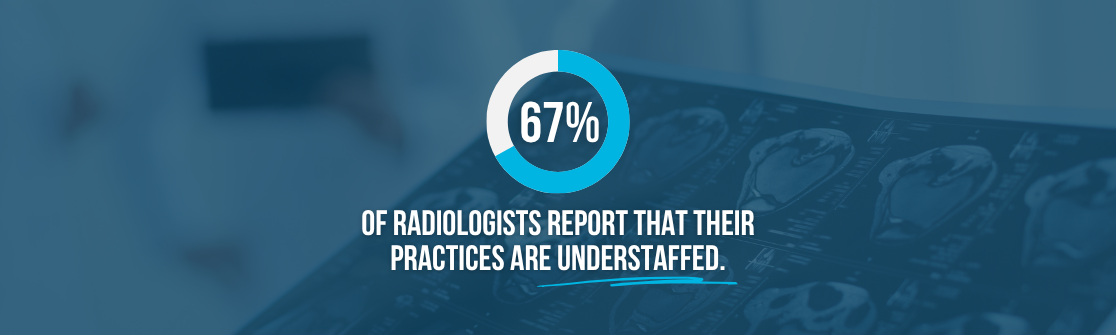
Radiology remains one of the most in-demand specialties in healthcare, but staffing it is becoming increasingly difficult. As the gap between imaging needs and the available radiologist workforce continues to grow, organizations are facing prolonged vacancies, delayed access, and rising pressure on existing teams.
To access the complete report on navigating the radiologist shortage, complete the short form below.
View the Full Radiologist Shortage White Paper Here:
View the Full Radiologist Shortage White Paper Here:
Radiology by the Numbers: Workforce & Job Growth Projections
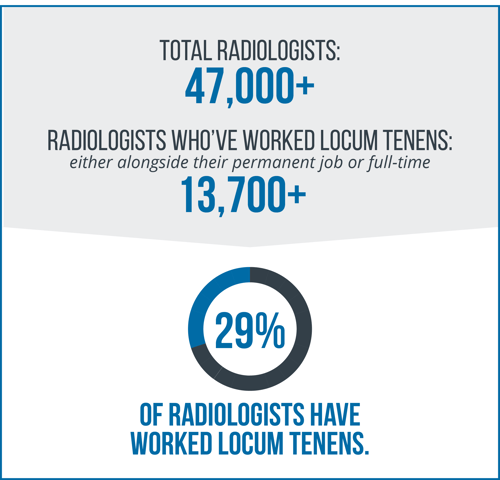
There are approximately 41,000 radiologists in the United States; however, workforce projections indicate that the supply of available radiologists will not be sufficient to meet the rising demand for care.
The U.S. Bureau of Labor Statistics predicts 4% growth in radiology from 2023 to 2033, resulting in 1,200 radiology job openings projected over that period.
Locum Tenens Radiology: Inside the Interim Radiology Workforce
According to the National Association of Locum Tenens Organizations (NALTO), more than 52,000 physicians work locum tenens annually.
As radiologist shortages persist, healthcare organizations are increasingly relying on locum tenens to maintain uninterrupted access to imaging and diagnostic services.
Key Drivers: Factors Contributing to the Radiologist Shortage
Limited Residency Positions: Slowing Growth in Radiology
Radiology is one of the most competitive medical residencies. Within interventional radiology residency, roughly 1 in 6 PGY-1 applicants will match; diagnostic radiology is even more challenging, with approximately 1 in 7 PGY-1 applicants anticipated to match, based on data from the National Resident Matching Program (NRMP).

Despite the strong interest in radiology, without an increase in available residency positions, the demand for radiologists is expected to outpace the supply.
Burnout & Attrition: A Growing Threat to Staffing Stability
Burnout remains a major concern for radiologists. According to the American College of Radiology, the volume of images and the complexity of each study have grown substantially, making interpretation more time-intensive and challenging for radiologists.

Additionally, since the COVID-19 pandemic, the annual attrition rate among radiologists has increased substantially.

Together, continuous burnout and rising attrition rates are weakening radiology workforce stability and making it more difficult for hospitals, healthcare facilities, and groups to meet demand.
Actionable Strategies: Addressing the Rising Demand
Adopt Teleradiology: Expanding Access to Radiological Care
Teleradiology is emerging as a scalable solution for managing radiologist shortages. Enabling remote image interpretation allows health systems to maintain radiology coverage across regions, even when local radiology staffing is limited.

Teleradiology's rapid adoption is being driven not only by operational need but also by its potential to reduce burnout and improve retention among radiologists.

As health systems navigate rising demand for radiologists, teleradiology offers a sustainable way to maintain high-quality coverage across geographic and staffing constraints.
Utilize Locum Tenens Radiologists: Bridging Gaps in Coverage
As radiology staffing challenges persist, utilizing locum tenens radiologists is a vital strategy for maintaining access to radiological care.

Utilizing locum tenens radiologists while partnering with a trusted locum tenens staffing agency like Medicus ensures reliable coverage and support. By managing the complexities of locum tenens staffing, Medicus provides the necessary resources and expertise to help maintain continuity of care while minimizing the strain on permanent teams.
Frequently Asked Questions About the Radiology Workforce:
How Many Radiologists Are in the United States?
There are approximately 41,000 radiologists in the United States, with nearly 90% specializing in diagnostic radiology.
How Many Radiologists Work Locum Tenens in the U.S.?
According to Medicus' proprietary data, as of June 2025, an estimated 13,718 radiologists have worked locum tenens in tandem with their permanent job or as a standalone career.
What States Have the Fewest Radiologists Per Capita (100,000)?
The states with the lowest number of radiologists per capita include Nevada, Oklahoma, Mississippi, and Wyoming.
Why is There a Shortage of Radiologists?
The shortage of radiologists is due to a combination of factors, including an aging population, a limited pipeline of new providers, attrition rates, and other additional factors.
%20(2)%20(1).png)