The Physician Workforce Under Pressure: From Shortage to Strategy

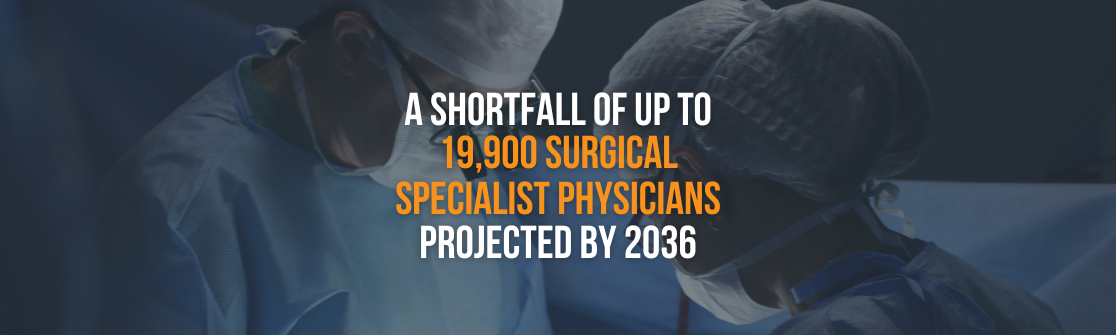
The physician shortage is reshaping how healthcare leaders think about access, capacity, and workforce strategy. With demand continuing to outpace physician availability, organizations are being forced to address not only immediate coverage gaps but long-term sustainability.
Access the Complete Report for a Comprehensive Look at the U.S. Physician Shortage
Access the Complete Report for a Comprehensive Look at the U.S. Physician Shortage
By the Numbers: Physician Workforce & Job Growth Projections
There are over 1 million physicians in the United States, though workforce distribution and availability vary significantly by specialty and region.

Looking ahead, physician employment is expected to grow steadily. The U.S. Bureau of Labor Statistics projects 3% job growth from 2024 to 2034, translating to roughly 24,300 openings over the next decade as demand continues to rise.
Locum Tenens Physicians: An Inside Look at Interim Healthcare Workforce
An estimated 165,000 physicians have engaged in locum tenens work at some point in their careers, reflecting a fundamental shift in how care is delivered amid persistent workforce constraints.

Pediatrics, OB/GYN, and surgery also see high locum tenens utilization rates, reflecting an ongoing reliance on interim coverage to maintain continuity of care.
Key Drivers: Factors Contributing to the Physician Shortage
An Aging Population: Increased Demand for Healthcare Services
Demographic shifts, particularly the aging population, remain one of the primary drivers behind the increasing demand for physicians.
An Aging Physician Workforce: Implications for Future Capacity
Rising care demands from an aging population are converging with an aging workforce, intensifying physician shortages.
With nearly half of the physician workforce expected to retire over the next decade and rising demand from an aging population, the resulting supply-demand imbalance is likely to intensify, creating greater operational strain for healthcare teams and organizations.
Limited Training Opportunities: A Supply & Demand Mismatch
Despite modest growth in residency positions, the gap between the number of applicants and available training slots persists.
As a result, many medical graduates face delays starting residency, which limits the rate at which new physicians enter the field and reduces the pipeline needed to meet rising patient demand.
Patient & Operational Impact: Effects of Provider Shortages
Geographical Disparities: Disproportionate Access to Care
Even as projections indicate a growing physician shortage ahead, the gap is already significant when considering access disparities.
Several high-demand physician specialties illustrate how geographic disparities can translate into measurable access gaps and increased travel time for rural patients.

These access gaps exist alongside broader structural challenges in rural healthcare. Over the past decade, more than 100 rural hospitals have closed, leaving many communities without emergency, inpatient, and essential hospital services.
Hospital Closures & Service Line Reductions: Loss of Local Patient Access Points
Hospital closures and service line reductions are increasing nationwide. As inpatient and specialty services are reduced or consolidated, patients face longer travel and wait times for appropriate treatment, often delaying care until conditions become urgent.
This elevated closure risk among U.S. hospitals is already shaping service line availability, with certain specialties experiencing disproportionate impacts as hospitals scale back or eliminate care offerings.
Actionable Strategies: Navigating the Physician Shortage
Invest in Care Team Models: Integrating Advanced Practice Providers
Care team models that integrate advanced practice providers (APPs) offer a scalable strategy to expand capacity without overextending physicians.

By distributing care tasks across a multidisciplinary team, care team models enhance patient throughput, maintain clinical quality, and enable physicians to focus on higher-acuity or procedure-based care.
Prioritize Culture: Strengthening Recruitment & Retention
Physician workforce stability is increasingly influenced by organizational culture, underscoring its role in long-term recruitment, retention, and workforce planning.

Build Contingency Plans: Ensuring Operational Continuity
Contingency planning provides healthcare organizations with a proactive approach to maintaining stability with ongoing physician shortages.  With physician vacancies taking an average of 224 days to fill, a well-designed contingency plan ensures immediate coverage when gaps occur.
With physician vacancies taking an average of 224 days to fill, a well-designed contingency plan ensures immediate coverage when gaps occur.

Leverage Locum Tenens: Bridging Gaps in Coverage
As physician shortages continue to heighten, implementing locum tenens into staffing strategies can help maintain access to care and stabilize coverage across nearly all specialties.

Partnering with a trusted locum tenens agency, such as Medicus, provides access to qualified providers and streamlined staffing support, allowing leaders to focus on long-term workforce planning while ensuring seamless, sustainable day-to-day coverage.
For a comprehensive overview of the factors driving the United States physician shortage and actionable strategies leaders can use to maintain access to care, view the complete report here.
Frequently Asked Questions about the United States Physician Shortage
Why is There a Physician Shortage in the U.S.?
The United States physician shortage is due to a combination of factors, including demographic shifts such as an aging population and workforce, training bottlenecks, and physician burnout.
Which States Have Physician Shortages?
While physician shortages are present in nearly every state, their effects are more pronounced in rural areas than in urban areas.
How Many Physicians Are in the United States?
There are over 1 million physicians in the U.S., with exact numbers varying by specialty.
How Many Locum Tenens Physicians Are There in the United States?
According to the National Association of Locum Tenens Organizations (NALTO), around 52,000 physicians work locum tenens each year.
How to Solve the Physician Shortage?
The physician shortage reflects a complex set of challenges, and no single strategy fully addresses it. Efforts often center on increasing training capacity and rethinking how care teams are structured. Additional approaches include broader use of advanced practitioners, targeted support for underserved communities, and locum tenens coverage to help sustain patient access.