Closing the Distance: Rural Physician Shortages & the Role of Locum Tenens

Rural America is home to nearly 61 million individuals, yet many communities face widening gaps in access to essential healthcare services. Hospital closures, staffing shortages, and limited specialty resources have created new pressures for leaders working to safeguard patient care.
As these challenges intensify, many healthcare organizations are increasingly turning to locum tenens as one solution that helps maintain access to rural healthcare.
Understanding the Challenges Facing Rural Healthcare
Rural Hospital Closures
Over the past decade, more than 100 rural hospitals have closed, leaving many communities without access to emergency services, inpatient care, and essential hospital services. Financial instability now places more than 700 additional hospitals at risk of closure, including approximately 300 that the Center for Healthcare Quality and Payment Reform classifies as being at immediate risk of closure.
While closures are occurring nationwide, several states face higher concentrations of hospitals at immediate risk as of October 2025, including Connecticut (50%), Alabama (48%), Mississippi (34%), New York (31%), and Kansas (30%).

Physician Shortages & an Aging Workforce
Physician shortages affect the entire country, but the impact is felt more acutely in rural communities where provider-to-resident ratios are already lower. Rural areas average about 30 physicians or specialists per 100,000 people compared to 263 in urban areas, which reduces access to both primary and specialty care.
Training patterns also contribute to physician shortages in rural areas. Data from the Association of American Medical Colleges (AAMC) shows that nearly 60% of physicians practice within the state where they completed residency. With the vast majority of residency programs in urban areas, fewer physicians ultimately enter practice in rural communities.
At the same time, the rural physician workforce is aging. More than half of rural doctors aged 50 or older are expected to retire by 2030, resulting in a projected 23% decline in rural physicians. As retirements accelerate and fewer trainees begin their careers in rural areas, many communities face a shrinking supply of local physicians.
Limited Specialists & Increased Travel Times
Rural communities face a disproportionate shortage of physicians, specifically specialists. Shortages span multiple disciplines, with notable gaps in:
- Primary Care: Approximately 66% of designated primary care Health Professional Shortage Areas are located in rural areas, according to findings by the National Center for Health Workforce Analysis.
- Emergency Medicine: Approximately 1 in 13 U.S. emergency departments lacks 24/7 attending physician coverage, according to data published in the Journal of the American College of Emergency Physicians Open.
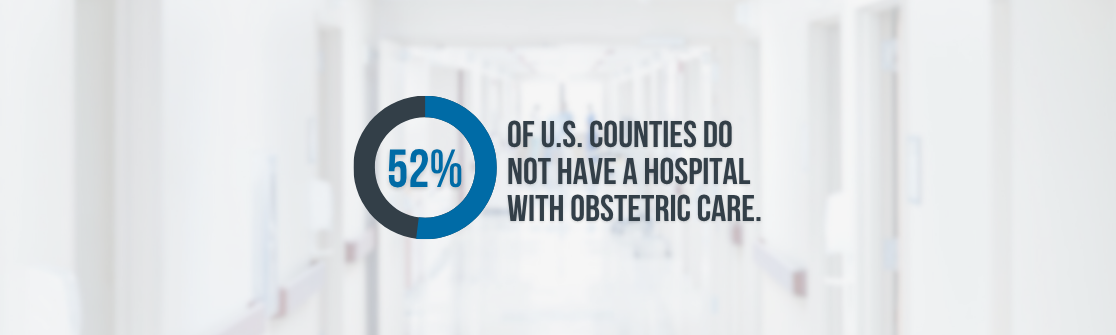
- OB/GYN: Over half of U.S. counties do not have a hospital with an obstetric unit, according to the March of Dimes.
- Psychiatry: Currently, only 26.4% of the existing need for psychiatric care is being met by psychiatrists, according to findings reported by the Kaiser Family Foundation (KFF).
- Gastroenterology: 69.3% of counties within the U.S. do not have an active gastroenterologist, according to research published in Gastroenterology.
As shortages grow, rural residents often travel long distances for routine care, diagnostic testing, and specialty consultations. On average, they travel more than twice as far for medical services compared to individuals in urban areas.
These shortages also extend to emergency response. Rural emergency medical services may have response times almost 20 minutes longer than the national average, and transport times to specialty centers can exceed the national average by more than 40 minutes.
How Locum Tenens Helps Expand Rural Healthcare Access
As physician shortages, financial constraints, and ongoing closures continue to challenge rural hospitals and clinics across the country, many healthcare organizations are facing new questions about how to maintain access to care for the communities they serve. While these challenges are multifaceted, one approach to helping ease the pressures of rural healthcare shortages is locum tenens coverage.
The Role of Locum Tenens in Rural Healthcare:
- Helping facilities maintain coverage: Rural hospitals and clinics often rely on locum tenens when vacancies or staff absences would otherwise limit access to care. Locum support enables organizations to maintain operational continuity, preserve service lines, and ensure timely patient care.
- Expanding Access to Specialty Care: Many rural communities have limited or no local specialty resources. Bringing in locum tenens specialists enables patients to receive evaluations and procedures closer to home, which reduces travel burdens and helps organizations offer services that might not be sustainable on a permanent basis.
- Providing Stability During Recruitment: Recruiting permanent clinicians in rural areas takes time, particularly in high-demand specialties. Locum tenens coverage allows organizations to continue meeting patient needs while conducting a thoughtful search and onboarding process.
- Supporting Rural Care Teams: Smaller care teams often carry significant workloads. Seasonal demand, turnover, and persistent staffing gaps increase the risk of burnout and turnover. Locum tenens clinicians help share clinical responsibilities, give permanent staff space for time away, and provide greater flexibility around scheduling preferences.
- Building Sustainable Staffing Models: More healthcare leaders are incorporating locum tenens into long-term workforce planning to support clinical stability. For organizations managing multiple FTE gaps, the Medicus Transition Program helps stabilize health systems during periods of clinical disruption and staffing transitions.
Locum tenens physicians and advanced practitioners play an essential role in helping rural communities maintain access to timely care. Their support helps reduce wait times, strengthen continuity, and ensure that vital services remain available when permanent staffing is limited.
Recognizing National Rural Health Day
National Rural Health Day celebrates the dedication of healthcare organizations, providers, and community partners who work tirelessly to support rural populations. It also brings needed attention to the workforce challenges these communities continue to face. At Medicus, we are proud to partner with rural facilities by providing reliable locum tenens physicians and advanced practitioners who help maintain consistent access to care for the patients who depend on their local hospitals and clinics.
If you are interested in learning how Medicus can support your healthcare facility with locum tenens staffing, click here or complete the short form below to connect with a member of the Medicus team.