Becker's Hospital Review: How The Medicus Transition Program Restores Workforce Stability
Healthcare organizations across the country are feeling the weight of clinical workforce shortages. As a result, many are struggling to keep pace with patient demands—some operating at reduced capacity simply because they can’t fully staff their services. With providers stretched thin and burnout on the rise, traditional staffing models can’t keep up with the pace or complexity of today’s challenges.
At a time when quick fixes fall short and the pressure to maintain care quality remains high, how can healthcare leaders drive sustainable staffing outcomes? A recent Becker's Hospital Review article explores how three health systems successfully addressed these challenges by leveraging the Medicus Transition Program, a project-based interim healthcare staffing solution designed to help stabilize clinical workforces.
Reducing a 40,000-Case Radiology Backlog
A Michigan health system faced severe radiologist shortages across multiple facilities, leading to a 40,000-case imaging backlog and wait times exceeding 40 days. The strain on operations and patient care made an immediate solution critical.
The Medicus Transition Program Impact:
- Identified and onboarded 41 locum tenens radiologists who received temporary privileges in as little as one week.
- Scaled locum tenens staffing with 10 FTEs placed in 8 weeks to 20 FTEs within 3 months.
- Reduced the health systems 40,000-case backlog to just 3,500 cases in 5 weeks.



With the backlog cleared, patient wait times decreased, and radiology services stabilized, allowing the hospital to regain control over its operations. Read the entire radiology case study here.
Stabilizing OB-GYN Services to Meet Demand
A New York health system experienced sudden OB-GYN turnover, leading to disruptions in care and financial strain. To maintain services and ensure continuous access to women's health and prenatal care, leadership needed to secure immediate coverage.
The Medicus Transition Program Impact:
- Recruited and onboarded 20 locum tenens OB-GYNs and CMNs within 45 days.
- Increased delivery volumes by over 24% compared to the previous year.
- Secured permanent placements through Medicus' recruitment partner, Optimum.



Through the Medicus Transition Program, the hospitals secured continuous OB-GYN coverage and access to patient care and built a more cost-effective staffing model by adopting an OB-hospitalist staffing model. Explore the complete case study here.
Improving Surgical Access with an Anesthesia Care Team Model
An Illinois health system struggled with anesthesia staffing shortages, leading to surgical delays, a growing backlog, and patient redirections to other hospitals. With only 70% of ORs operational, leadership needed a sustainable solution to restore capacity and efficiency.
The Medicus Transition Program Impact:
- Onboarded and credentialed 150 locum tenens CRNAs and anesthesiologists in 60 days.
- Increased OR utilization from 70% to 100%.
- Assisted the health system transition from an outsourced MD-only staffing model to an employed anesthesia care team model.
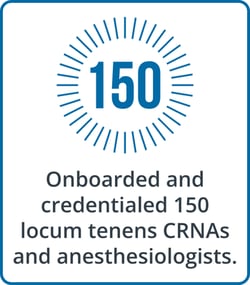


With full OR functionality restored, the hospital improved surgical access, enhanced workforce reliability, and adopted a sustainable staffing model. Read the complete anesthesia case study here.
A Proven Approach to Clinical Workforce Stabilization: The Medicus Transition Program
As health systems continue to face provider shortages, the Medicus Transition Program provides a strategic, consultant-based approach to stabilizing clinical workforces. By combining expert resources with flexible support, Medicus helps health systems maintain continuity of care, improve efficiency, and ensure high-quality patient care amid multi-FTE shortages.
To learn more about how these health systems turned workforce challenges into opportunities, read the complete Becker's Hospital Review article here.
.png)