The Latest Locum Tenens News & Trends
Connect with Medicus
Unlocking Career Independence: Embrace the Freedom of a Locum Tenens Career
Debunking the Myths: Unveiling the Reality of a Fulfilling Locum Tenens Career
Stabilizing Oncology Care: The Impact of a Medicus Locum at a Maine Medical Center
What States Can Nurse Practitioners Practice Independently?
The Anesthesia Provider Shortage: Confronting the Growing Demands for Care
Top Locum Tenens Destination: Michigan
We Asked the Experts: Best Tips for Integrating Locum Tenens Into Your Healthcare Facility
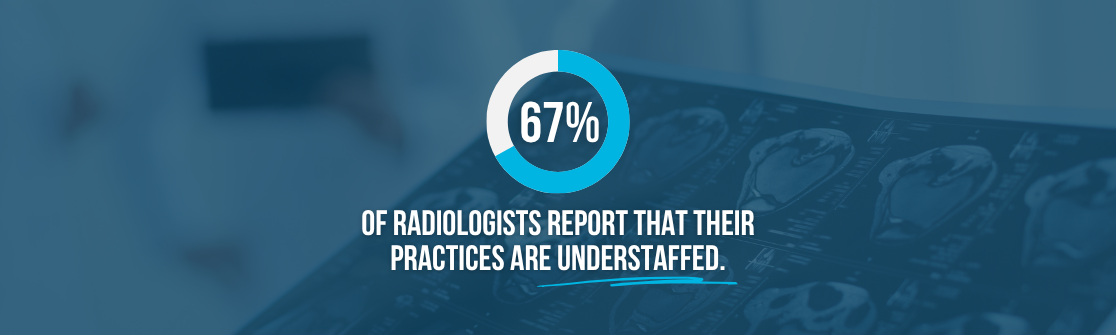
Navigating the Radiologist Shortage: Strategies for Meeting the Rising Demand in Healthcare
Planting Seeds of Change: How Medicus is Caring for People and the Planet
Closing Provider Shortages: Lessons in Building a Sustainable Clinical Workforce
Connect with Medicus

The Anesthesia Provider Shortage: Confronting the Growing Demands for Care

Exploring the Rising Demands in Emergency Medicine
Closing Provider Shortages: Identifying the Drivers of Clinical Workforce Shortages

Healthcare Market Report | Q2 2025

Healthcare Market Report | Q1 2025

2025 Healthcare Trends: Insights for Physicians and Advanced Practitioners

2025 Healthcare Trends: A Guide for C-Suite Executives